Researchers at Westlake University in Hangzhou have identified a potent “super antibody” capable of completely protecting mice from a lethal dose of a deadly tick-borne virus and slashing viral loads in primates by 90% within 24 hours. Led by structural biologist Dr. Tian Xingshan, the breakthrough targets Severe Fever with Thrombocytopenia Syndrome (SFTS)—a disease with a fatality rate up to 30%—and could pave the way for the first specific antiviral therapy against this growing threat.
Imagine a tick bite so dangerous it can lead to a fever, a catastrophic drop in platelets, and organ failure, with no targeted drug to stop it. That’s the grim reality for patients diagnosed with Severe Fever with Thrombocytopenia Syndrome (SFTS), a disease first identified in rural China in 2009. While Lyme disease dominates Western headlines, SFTS has been quietly spreading, carried by ticks whose habitats are expanding due to climate change. But now, a team at Westlake University might have found a key to fighting back, reported by the South China Morning Post.
This isn’t about a new vaccine just yet. The core innovation is a monoclonal antibody therapy designed to tackle the most critical problem in SFTS infection: uncontrolled viral replication that can overwhelm the body before the immune system mounts an effective defense. In simple terms, it stops the virus in its tracks.
The hunt for this defender began where you might expect: in the blood of survivors. The research team, collaborating with Zhoushan Hospital in a high-risk coastal region of Zhejiang province, screened tens of thousands of antibody candidates from recovered patients. Their search zeroed in on one extraordinarily effective protein, which they named ZS1C5.
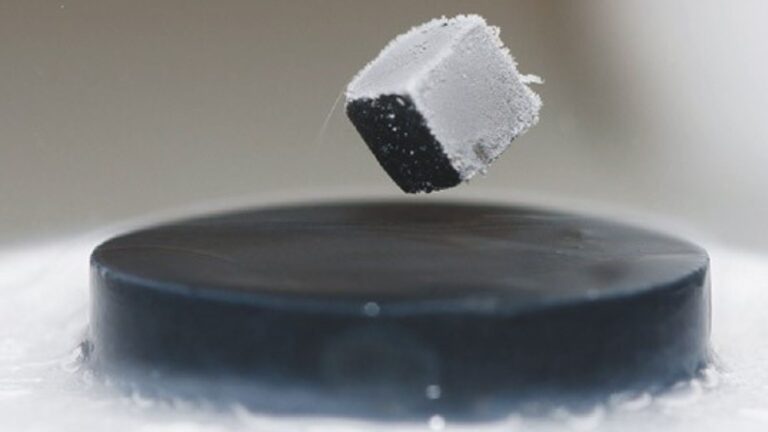
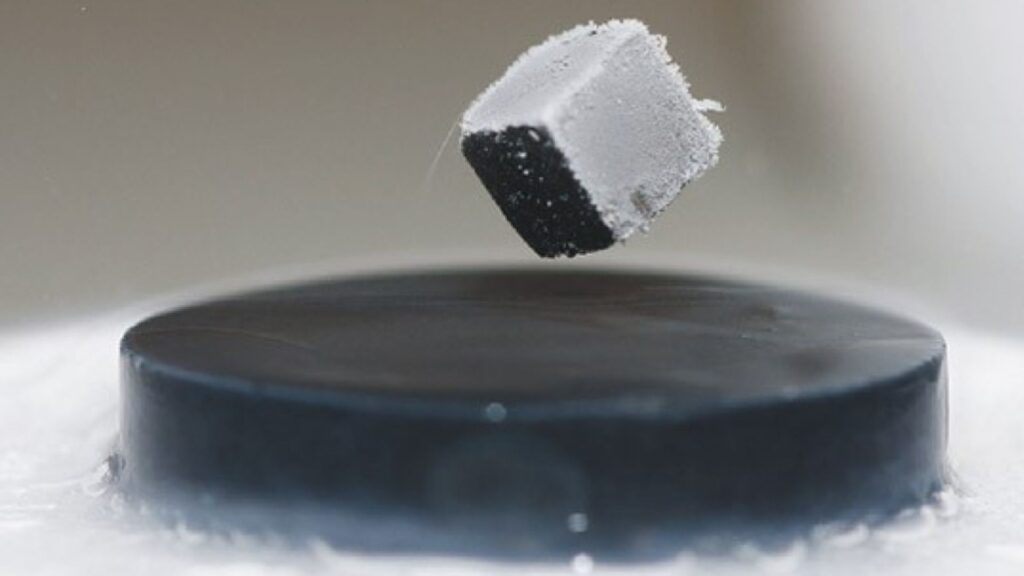
So, what does this antibody actually do? Think of it as a precision-guided molecular clamp. Using advanced structural biology, the team discovered that ZS1C5 possesses an ultra-long binding loop—a rare structural feature. This “arm” simultaneously latches onto two critical sites on the virus’s surface glycoprotein. This dual grip is the secret. It physically blocks the virus from attaching to human cells and also prevents the shape-shifting it needs to fuse with and invade them. It neutralizes the threat outright.
The laboratory data was compelling, but the real proof came from animal trials, a critical step reported by the SCMP. In mice given a viral dose ten times the lethal amount, a single injection of ZS1C5 resulted in a 100% survival rate. Remarkably, it remained effective even when administered 48 hours after infection. In rhesus monkeys, which closely model human disease, the results were just as striking. Viral loads in the blood plummeted by 90% within a single day and became undetectable within three days. Crucially, platelet counts—which crash in SFTS patients—remained stable.
WATCH ALSO: https://modernmechanics24.com/post/boston-dynamics-atlas-balance-agility/
The scientific vision to pursue this pathogen came from the research team at Westlake University, with structural biologist Dr. Tian Xingshan playing a leading role in deciphering the antibody’s unique mechanism. The engineering—the painstaking work of screening, isolating, and testing this candidate—was carried out by a collaborative team of virologists, immunologists, and clinicians from Westlake and their hospital partners in Zhejiang.
The potential impact here is profound. Currently, treatment for SFTS is purely supportive, often requiring lengthy, expensive stays in intensive care units with plasma exchange therapy. A targeted, effective antibody therapy could transform patient outcomes, reducing mortality, shortening severe illness, and alleviating the burden on healthcare systems. As one researcher noted, its cost would likely be far lower than complex ICU care.
Of course, a significant boundary remains. While the primate data is exceptionally promising, ZS1C5 has not yet been tested in human clinical trials. The journey from successful animal studies to an approved, commercially available therapeutic is long, expensive, and carries the inherent uncertainty of how human physiology will respond. Furthermore, while treatment is a major leap, prevention via a vaccine is still a separate, ongoing challenge.
READ ALSO: https://modernmechanics24.com/post/hku-ucla-decode-space-battery-mechanism/
The team’s next goal, following their January publication in the journal Vita, is to develop a vaccine that teaches the human immune system to produce antibodies like ZS1C5 on its own. The threat driving this urgency is expanding. The primary tick vector, Haemaphysalis longicornis, has now been found in the United States, Australia, and New Zealand. Human-to-human transmission through bodily fluids is also possible, as noted in a recent Lancet commentary. This makes the work at Westlake University not just a regional advancement, but a crucial step in preparing for a wider global health challenge.